The story of an abortion at 27 weeks, told two ways.
I first heard from Kristyn Smith in December of 2021. After discovering my podcast, ACCESS, she sent me an email with the subject line, “Abortion at 27 weeks.” In the email, she recounted a story of pregnancy complications that led her to the emergency room of a West Virginia hospital, where she encountered Dr. Byron Calhoun.
Calhoun is a nationally-known anti-abortion figure. Caroline Kitchener of The Washington Post had published an article about him about a month before Kristyn had the misfortune of ending up in his care. He believes that abortion is never necessary to save the life of a pregnant person, a fringe position even among anti-abortion OBGYNs, and he is the only high-risk obstetrician in Charleston, West Virginia. Despite a fatal fetal diagnosis and bleeding—which one other expert described to me as an “obstetric emergency”—Calhoun would not help Kristyn terminate her pregnancy. In the end, she had to drive six hours to Washington, D.C., bleeding all the while, in order to have an abortion.
But things went wrong in Kristyn’s story long before she met Calhoun. Her pregnancy was a desired one, but at her 20 week ultrasound, she received a diagnosis almost certain to be lethal: A small piece of tissue was obstructing the flow of urine out of her baby’s bladder. One thing I think a lot of people don’t know about pregnancy is that amniotic fluid is made mostly of fetal urine. (That’s right, fetuses swim around in their own pee.) This fluid is vital to fetal development in many ways, but particularly crucial for lung development. According to experts I spoke with, anhydramnios—meaning very little to no amniotic fluid—is the most universally agreed-upon lethal fetal diagnosis.
According to the American College of Obstetricians and Gynecologists, when a patient receives a diagnosis of this nature, their doctor should present all options to them. That includes terminating the pregnancy. But Kristyn’s doctors in West Virginia never even mentioned abortion. They immediately referred her to a hospital in Cincinnati, a three-and-a-half hour drive away, for fetal surgery. Even if this surgery had succeeded, her baby would have been born extremely sick. It failed. At this point, the Ohio doctors did talk to Kristyn about abortion, but they couldn’t actually offer her one, because she was past the legal point of termination in the state. They sent her home to wait for a stillbirth, a horrible proposition.
A midwife told Kristyn about Dupont Clinic, a Washington, D.C., practice that specializes in later abortion care. She made an appointment, but before the date arrived, she started bleeding and had to go to the hospital. There, Dr. Calhoun accused her of using drugs and repeatedly refused to help her terminate her pregnancy. She did eventually make it to D.C. for her abortion, but only because she took matters into her own hands and checked herself out of the hospital.
I know that a lot of people reading this story will think, “Well, of course that happened in West Virginia. It’s a red state.” But the truth is, the same thing would have happened to Kristyn at many hospitals in the U.S., regardless of the state, because many hospitals have their own anti-abortion policies. Catholic hospitals in particular limit abortion care to a dangerous extent, but many Protestant and secular hospitals do, as well. In fact, one Virginia abortion provider who works in an outpatient clinic told me that she is routinely referred complicated cases that would be better managed in hospitals, simply because doctors in those hospitals either can’t or won’t perform abortions.
As I got to work on a podcast episode examining how these anti-abortion doctors and facilities put pregnant people in danger, I knew there was another important angle to cover here: We’re about to see many more Kristyns. When the Supreme Court overturns Roe, within a year or two abortion will be banned in roughly half the country. The people living in those states will have to travel long distances and overcome tremendous logistical hurdles in order to get abortions. This will delay them, pushing them later into pregnancy, which means their abortions will be more expensive and much harder to get. Already, few abortion clinics offer procedures in the second trimester, let alone the third.
Last week, after many months of work, both versions of the story went live: on ACCESS, an examination of anti-abortion doctors and hospitals. Online and in print in The Nation, a look at what Kristyn’s story tells us about our post-Roe future. I was fortunate to receive a grant from the International Women’s Media Foundation’s new Reproductive Rights Reporting Fund to help me finish up the project.
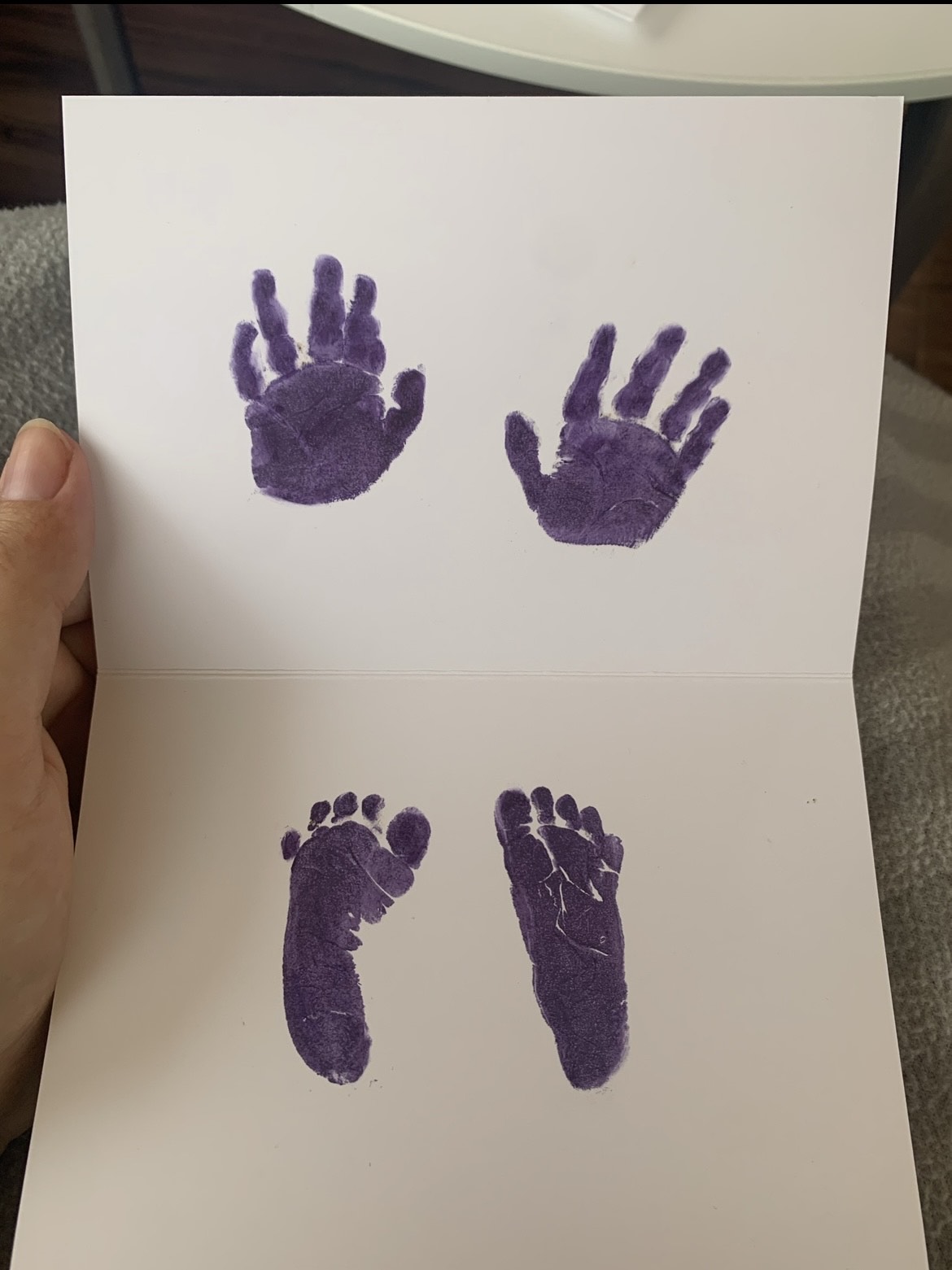
I want to end by acknowledging Kristyn’s bravery. Much of her family is opposed to abortion, and she also feared retaliation from a powerful doctor and hospital. She came forward anyway. Not only that—she relived some very traumatic experiences in our interview, and then fielded dozens of follow-up questions from me, and had to dig through all her medical records in the fact-checking process. It’s really, really hard to be a source for a story like this. I hope you’ll honor Kristyn’s bravery by reading and listening.



